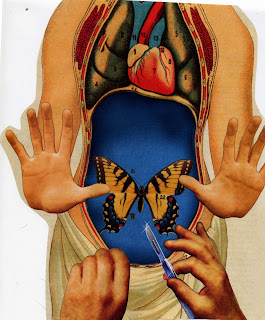
Your doctor has recommended a HYSTERECTOMY don't make a decision until you read this startling report on the real risks of surgery and the LESS-INVASIVE alternatives your ob-gyn may not be mentioning
IF SOMEONE suggested that you undergo an elective procedure that could keep you out of work- and in pain- for six weeks, might leave you incontinent, deep-six your sex life, increase your risk of osteoporosis and heart disease, and possibly shorten your life span, would you do it? Maybe not- but what if your trusted ob-gyn told you it was a good move? Chances are you would agree to it. In fact, every day, as often as 11 times every 10 minutes, women in the United States struggling with non-cancerous and heavy periods- agree to resolve the problem by getting rid of their reproductive organs. Ninety percent of hysterectomies in this country are performed for reasons other than cancer treatments, and the vast majority involve major open abdominal surgery. Where these women advised on alternatives, for example, detox programs to reduce toxic build up in liver, uterine lining, did they explore acupuncture to reduce pain, bleeding, perhaps,
Women between 40 and 54 are most at risk, and not just because the onset of many pelvic disorders occurs during the years leading up to menopause, The hysterectomy rate is so high because many of us take our doctor's word that once we are finished bearing babies, it's no great loss if our problematic uterus, and maybe even our ovaries, are removed. Don't believe it. And don't believe that there are no alternatives to hysterectomy. The question is, why isn't your doctor telling you about your options, alternatives.
WHY THE UTERUS IS WORTH KEEPING
EVIDENCE IS GROWING that our reproductive organ serve a purpose beyond birthing babies. In 2005 a landmark study showed that removing ovaries, which is still done during most hysterectomies to reduce the relatively small risk of ovarian cancer, actually increases the risk of heart disease and osteoporosis, according to a study coauthor William Parker MD, of UCLA School of Medicine.
While the ovaries produce a diminishing level of estrogen after you turn 45, for decades they will continue to produce testosterone and androstenedione, hormones that convert to estrogen when they circulate through out the body. These provide crucial protection against heart disease and osteoporosis. Testosterone also helps preserve our sex drive, bolster energy levels and maintain lean body mass, tissue. Even though some women opt to keep their ovaries when they undergo a hysterectomy, within four years of the operation about 15% will experience post operative ovarian failure, which triggers premature menopause.
All of this might be acceptable if doctors had no alternatives to offer women suffering from non-cancerous pelvic disorders. But that is far from the case. Over the past two decades, there has been a virtual explosion of new ways to treat pelvic problems. Laproscopic technology now allows ob-gyns to remove endometriosis and accompanying scar tissue, as well as fibroids, without cutting open the abdomen. Uterine artery embolization (UAE), which is performed through a minor incision in the groin, can shrink fibroid by cutting of their blood supply. Endometrial ablation, an out-patient procedure, can end bleeding by destroying the uterine lining via vaginal probe. Pessaries-which are diaphragm-like devices -and other fixes can lessen pain by lifting a fallen uterus back into place rather than removing it. Birth control pills, the progesterone IUD and other non-surgical therapies have also been shown to relive disabling pain and bleeding while leaving the uterus intact. Have your doctor let you know that alcohol consumption, diet and lifestyle changes can be the solution before other therapies are suggested. The uterus is related to the function and toxicity of the liver as well, if you have a clean, non toxic liver more likely that you are free from blood clots and pain.
"it is true that many of the new treatments may not be a permanent solution, more likely lifestyles, habits need to be of permanent changes.
"But many pelvic disorders naturally subsides as women get closer to menopause, after which recurrence is less likely" in other words , midlife women don't necessarily need a permanent solution: we just need a bridge treatment that can relive symptoms of non-cancerous pelvic conditions until we reach menopause.
Many of these treatments have existed since 1980s, which is why it's appealing that the annual rate of nearly 600,000 hysterectomies in U.S. hasn't declined significantly in 10 years, according to the Centers for Disease controls statistics. What is more, almost 70% of these hysterectomies are still being performed via open abdominal surgery, which was pioneered in 1843, despite the fact that laproscopic hysterectomy, available since the mid-to late- 1990s, is a less-invasive removal method. The surgery is guided by a tiny camera inserted into the body via a small incision, in a procedure that causes less pain, less scarring and less risk of infection. And women who have laproscopic surgery are back at work in about one third of the time as those who undergo an open abdominal hysterectomy.
with such effective alternative now available, why do physicians continue to treat non-life-threatening problems by removing our reproductive organs? why, even when hysterectomy is appropriate for non-cancerous conditions, is it being done in the most scarring and disabling way possible? and why are we-a generation of women who research and challenges personal trainers, investment advisers and other professional is our life-allowing this?
When Hysterectomy May be the Answer
If you have been diagnosed with uterine, cervical, ovarian or one of the other cancers affecting the pelvic region a hysterectomy can stop the spread of disease and may save your life,
If your uterus hemorrhages or ruptures during or after child birth,
If you have severe, intractable bleeding that does not respond to a variety of non0-surgical, less invasive therapies, " In the vast majority of cases, however, bleeding can be controlled "
If you have been diagnosed with adenomyosis, buildup of endometrial tissue that invades the uterine wall, hysterectomy might provide pain relief ( endometriosis alone, even when it is extensive, rarely need surgery when treated with alternatives, acupuncture, nutrition, lifestyle changes, detoxification"
If your uterus has prolapsed and is falling out of your body through your vagina. however you should first try less drastic measures, such as using a pessary or having corrective surgery, and resort to hysterectomy if all other treatments fail.
How to find alternative treatment
www.catherinecoudray.com
healthywomen.org
mayoclinic.com/health/uterine








